Auto Deploying EpiPen that reacts to anaphylactic symptoms
Grade 8
Presentation
Problem
Problem and Solution
Problem: An epipen has to be used in an anaphylactic reaction. Sometimes when the reaction is too severe, you are not able to use the Epipen so someone near you has to insert the Epipen in your body for you. The problem is not a lot of people use Epipens or are educated on how to use them so people don’t know what to do if you are having an anaphylactic reaction.
Solution: To solve this problem we decided to design a device that inserts epinephrine when anaphylactic symptoms are detected.
Method
Introduction
Every year, people of all ages and backgrounds experience allergies. While most allergies are not severe, some can be life-threatening. When people are extremely allergic to certain things, they are at risk of an anaphylactic reaction which, if left untreated, can lead to death. Luckily, we have a solution to this problem: a new and innovative design for an EpiPen, which we have named the EpiPump!
This person has taken an allergy test, with the numbers in the picture showing different areas that the nurse testing them pricked and put suspect allergens on top of. Raised bumps can be seen, as a mild reaction.
Source: “Food allergies.” WikiLectures, 1 November 2023, https://www.wikilectures.eu/w/Food_allergies. Accessed February 25, 2024.
What are allergies and what is anaphylaxis?
Allergies are a mistaken reaction your immune system makes when it thinks it needs to defend your body, even if the substance it’s defending against is harmless. Though allergies can result in symptoms like rashes, hives, eyes watering, etc, it doesn’t always cause much harm to you. But, there is one exception. Anaphylaxis is a life-threatening reaction that occurs when an allergen comes into contact with a person. The allergen is usually the most common allergens such as shellfish, peanuts, milk, soy, eggs, etc. If not treated quickly, then the person can die.
Source: “Autoimmune urticaria.” Wikipedia, https://en.wikipedia.org/wiki/Autoimmune_urticaria. Accessed February 25 2024.
“Pink Eye/Conjunctivitis — Trailhead Pediatrics.” Trailhead Pediatrics, https://www.trailheadpediatrics.com/pinkeye. Accessed February 25 2024.
Symptoms and signs of anaphylaxis
Mast cells are responsible for releasing histamines in the body. Histamines are chemical hormones that can cause anaphylaxis, triggering the body to react to harmless substances. This reaction can result in redness, inflammation, hives, and rashes. The histamines enter the bloodstream when they are ejected from the mast cells, causing the arteries near the site of release to dilate. This sudden widening of the circulatory organ can lead to a sudden drop in blood pressure, which can be life-threatening. Due to increased blood flow in the area, the skin at the site of release may appear red, thick, and swollen.
Source: “Anaphylaxis: Causes, Symptoms, Diagnosis & Treatment.” Cleveland Clinic, 17 October 2023, https://my.clevelandclinic.org/health/diseases/8619-anaphylaxis. Accessed February 25 2024.
How can Anaphylactic reactions be oppressed?
If you experience symptoms of an anaphylactic reaction, it is important to take an EpiPen as soon as possible. The EpiPen works by regulating the body's reactions to the allergen by lowering histamine levels. This will stabilize your condition and prevent further complications. After taking the EpiPen, it is recommended to lie down. This will help improve blood flow and restore your blood pressure to its normal state.
Source: “5 emergency steps - for treating anaphylaxis.” Food Allergy Canada, https://foodallergycanada.ca/wp-content/uploads/5-emergency-steps-for-treating-anaphylaxis.pdf. Accessed 25 February 2024.
What is an EpiPen and how does it work?
An EpiPen is a medical device that delivers a dose of epinephrine (also called adrenaline), which helps counteract the effects of histamine. Histamine is a chemical released by your body's mast cells when they react to an allergen. While your body will gradually release epinephrine, the EpiPen is used to speed up the process and help your body handle the after-effects of the allergy.
The EpiPen comes in two products: EpiPen and EpiPen Jr. EpiPen Jr contains a 0.15 mL dosage, while the EpiPen contains a 0.3 mL dosage. Weight also plays a part in which to use.
Source: “How EpiPen® works.” Epipen.ca, https://www.epipen.ca/how-epipen-works. Accessed 25 February 2024.
Design and Planning
Our design is similar to the function and appearance of an insulin pump. We had two designs, one of which we concluded could not function with our knowledge currently and the technology available to us for potential construction. Our final design was based on a tube insulin pump, with all the same features and functions, excluding two differences: our EpiPump would deliver a dose of epinephrine rather than a set rate of basal insulin, and sensors based on the insulin pump would rather be detecting symptoms of anaphylaxis instead of insulin decrease.
We changed our design due to some shortcomings within it. As said before, our previous design was meant to look and function similar to a tubeless insulin pump, but the knowledge we had limited the design we could make. A tube insulin pump was much more feasible in our eyes due to its less compact and small design and the way the parts and functions are spread out. Another setback we mentioned was with the technology available to us. Since tubeless insulin pumps are much smaller, their parts are laid out very densely and are not as spread out as tube insulin pumps. So, their parts would have to be much smaller. Since we have a smaller window of access to the parts we would require for that design, we dropped it and converted it into a tube insulin pump.
The tube insulin pump was much less compact, and its parts were spread out, opposing the tubeless insulin pump design.
Source: “File: Medtronic Paradigm 754.front.ajb.jpg.” Wikipedia, 2012, https://en.m.wikipedia.org/wiki/File:Medtronic_Paradigm_754.front.ajb.jpg. Accessed February 25 2024.
Design Idea
For the name of our innovation, we have decided to keep the name EpiPump, which resembles the functions of the innovation. Our innovation project is based on the combination of an insulin pump and an EpiPen. As said before in the previous slide, the Epi Pump will work as a normal insulin pump but is meant for patients experiencing anaphylaxis.
Source: “File:Adrenalina autoinyector1.JPG.” Wikimedia Commons, https://commons.wikimedia.org/wiki/File:Adrenalina_autoinyector1.JPG. Accessed 11 March 2024.
EpiPump Explanation and Warnings of Caution
If symptoms of anaphylaxis are detected such as high histamine levels or low blood pressure, the monitor would give out a signal to both your pump and to your phone. As the signal is received, the pump inserts the prescribed amount of epinephrine into your body, which should stabilize your condition.
The same steps should be taken if you were to use an EpiPen. You should lie down after your dosage and call 911 after taking any life-saving medication. If one dosage doesn’t help, then IMMEDIATELY call 911 for help, as the condition could get worse and become fatal. Always have caution when dealing with any allergies, especially anaphylaxis, as they are unpredictable and can become fatal at any time. As the EpiPump would do most of the work, the only job the patient has to do (which the pump will alert them to do) is to lie down or sit with their legs open.
Insulin Pump Diagram
As our Epi Pump resembles an insulin pump, it will also have most of the same internal parts as well. Most of the differences will come in the medicine and the dosage size, as well as the dosing container.
The EpiPump is based on two main designs: the tandem diabetes insulin pump (bottom image) for the hardware design, and the Ultra Low-cost insulin pump created by NIH.gov (top image) for the internal components. The EpiPump will detect the symptoms of the heart rate and immediate drop in blood pressure, as well as the activation of mast cells.
Source: “Design of an open source ultra low cost insulin pump.” NCBI, 15 November 2022, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9679028/. Accessed 25 February 2024.
Sensor Functions
The EpiPump will have 3 main components: the cannula and the needle, the pump, and the monitors. The monitors used in the EpiPump will be an optical heart sensor (the same Apple watch tech) and a chemical sensor to detect hormones that are released when anaphylaxis occurs (specific histamines in the body). The optical heart sensor works by using green flashing LEDs that get absorbed by the blood inside of your body. When the heart beats and more blood flows, the absorption of the green light is greater, and the light-sensitive photodiode sensors measure the amount of light reflected and absorbed. A chemical or fluorescent sensor would also be used to detect the amount of histamine or leukotriene neurotransmitters in the body. This could be done by sensors detecting chemicals exclusive to mast cells, like proteoglycans and proteases. The fluorescent sensor can also detect bioactive amines within the bloodstream.
LED’s (green, but red in the image)
Photodiode sensors
Infrared sensors
Source: “Histology, Mast Cells - StatPearls.” NCBI, https://www.ncbi.nlm.nih.gov/books/NBK499904/. Accessed 25 February 2024.
Karra, Laila, and Francesca Levi. “Mast Cell Biology: Introduction and Overview - PMC.” NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3398748/. Accessed 25 February 2024.
“Mast Cells – Cells and Smears.” Cells and Smears, 22 March 2018, https://vetclinpathimages.com/2018/03/22/mast-cells/. Accessed 25 February 2024.
“Monitor your heart rate with Apple Watch.” Apple Support, 21 September 2023, https://support.apple.com/en-ca/HT204666. Accessed 25 February 2024.
Surtini, Rusty. “,.” , - YouTube, 6 May 2021, https://pubs.acs.org/doi/10.1021/cr400546e. Accessed 25 February 2024.
Monitor area
The monitor can be placed above major arteries (aorta artery for optimal histamine detection). The aorta artery is located in the middle of the chest.
The sensor is to be placed near the chest, outer thigh (far from your infusion set), or outer arm.
Source: Smolinska, Sylwia. “Metabolites | Free Full-Text | Histamine: A Mediator of Intestinal Disorders—A Review.” MDPI, 10 December 1989, https://www.mdpi.com/2218-1989/12/10/895. Accessed 25 February 2024.
How the pump will work
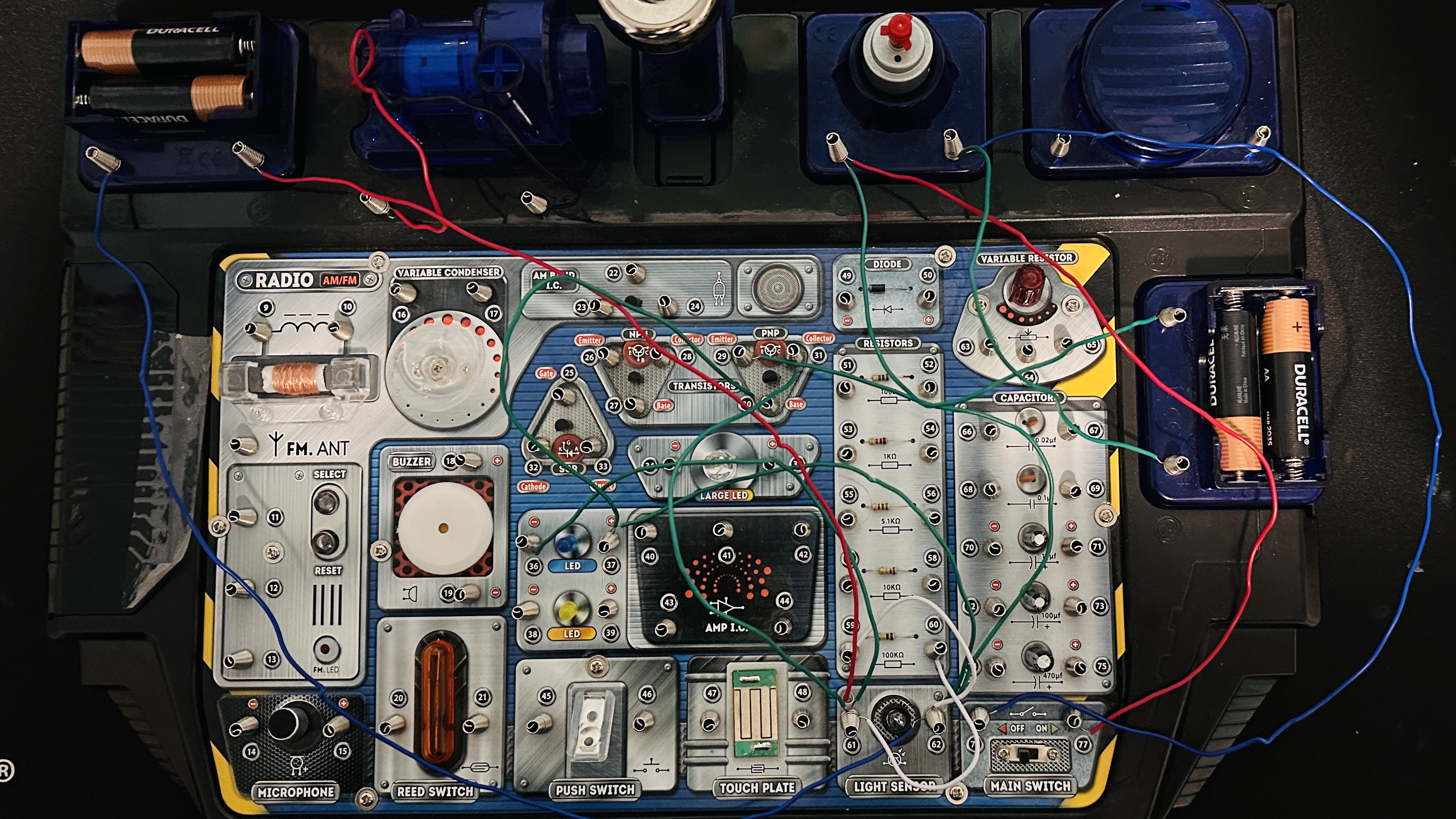
For the functions of the pump, it will require a PCB and some level of coding that will make the pump function. But apart from that, it will be the size of a small iPhone or pager (normal insulin pump size) that has the insulated dosage container on the top left corner. A rechargeable AA battery will be enough to power the Epi Pump. Note: The video link below shows how the pump will work through the use of an intuitive circuit board. It is just a demonstration of how we expect it to work. It does not symbolize the function of the PCB within the pump.
Link to how the EpiPump will work video.
Source: “Main parts of an insulin pump. | Download Scientific Diagram.” ResearchGate, https://www.researchgate.net/figure/Main-parts-of-an-insulin-pump_fig3_44853030. Accessed 25 February 2024.
How the pump will work continued
To start, the EpiPump will be monitored at all times when it is on, so battery depletion is going to happen quicker if the pump is on at times when there are little to no risk factors in activities. The sensors located on the chest will collect data at a set time that you can change manually through the pump buttons and settings. They will also send this data to the pump which will analyze and give the data to the patient through the pump screen in an intuitive graph showing the presence of histamines and the different blood pressures and heart rates at different times of the day. But, once the sensors detect the first signs of anaphylaxis (which are rarely ever wrong) the sensor will send the information to the pump, which the pump will use to activate the motor powered by the battery to dose the patient with epinephrine. This will stabilize their condition and normally end the reaction. Then, the device will call 911 and hospital transportation of the location of the patient will be arranged to be taken to the hospital.
The motor will work through the use of a PCB, code, and an AA battery. The motor will turn a gear which, in turn, will make a worm screw turn and push a plunger into the cartridge through the use of a piston. Once the medicine has been fully pushed into the cannula, the plunger will retract and the tubing can be removed from the cannula.
How the infusion set functions
The infusion set will be the usual cannula and the tiny needle protruding into the subcutaneous layer of the skin (underneath the epidermis and dermis) that will stay in place for usually ten weeks. The patch that holds the cannula needle in place on the middle outer thigh will have an adhesive mixture of both acrylic and silicone adhesives to maximize the strength and wear time of the cannula, while also ensuring that the cannula does not hurt the patient's skin when pulled out (time could range from 3-5 or 7 weeks based on the patient's activities). As for the tube itself, it will be about 10 to 24 inches in length to allow comfort when standing or sitting with the patient. The tubing can come in sizes varying by 2 inches each. When the cannula is connected to the patch on the patient's leg, the same clicking connection that insulin pumps have will be applied. This ensures that the patient will get the medicine properly and they can detach the EpiPump when doing tasks like swimming, exercising, or cleansing themselves.
The cannula needle will be 2 cm long. However, different needle lengths can be chosen for obese patients with more subcutaneous tissue for their health.
Source: Morse, Susan. “Home infusion company AxelaCare Health Solutions buys Ambient Healthcare.” Healthcare Finance News, 7 January 2015, https://www.healthcarefinancenews.com/news/home-infusion-company-axelacare-health-solutions-buys-ambient-healthcare. Accessed February 25 2024.
YouTube: Home, 23 December 2023, https://www.associazionemediciendocrinologi.it/images/eventi/congressi-nazionali/2019/Hands-on/1-TecnolDM/01_Misischi.pdf. Accessed 11 March 2024.
Procedure for changing Epinephrine cartridge
To change the cartridge of epinephrine after the dosage has been given, you must first remove the infusion set from the cannula to stop any accidental leaks in the tubing. You will require a new infusion set, new cartridge, syringe with needle, and 3 mL of epinephrine medication.
- First, set the pump to load mode, so that a new cartridge can be loaded without epinephrine entering the tubing. After the tubing has been removed completely, remove the current cartridge of epinephrine.
- Then, using the syringe, slowly and carefully pierce the container for the 5 mL of epinephrine on the top area meant for the needle.
- Then, slowly draw the medicine up through the needle until it is completely taken within the needle Turn the needle upright and flick the needle 5-10 times for any air bubbles in the medicine to be pushed to the top or popped.
4. Very slowly press on the needle, to release the air bubbles within the needle. Stop when you see the epinephrine coming out of the needle.
5. Once this step is complete, pierce the syringe into the storage area and slowly push the needle into the new cartridge.
6. Once that step is complete, cautiously and slowly push the medicine into the cartridge until it is FULLY complete.
7. Lastly, push the cartridge into its space within the pump using the guard ridges to guide you. Remember to also log the expiration date on the epinephrine container to allow for a reminder to change the cartridge if not used by the expiration. This step is complete.
Source: Reynolds, Roni. “How to Change Tandem Insulin Pump Cartridge and Infusion Set.” YouTube, 28 April 2021, https://www.youtube.com/watch?v=ZcQB2Ql90Ik. Accessed 11 March 2024.
Procedure to change infusion set
If the Infusion set connected to your body falls off or gets damaged, it is a sign that it is time to replace it.
Step 1: You first have to remove the tubing from the cannula. Depending on when you last changed the cartridge, you can either replace the whole infusion set if you're about to change your cartridge or change it in the next 12 hours. If you just changed your cartridge and the cannula falls off, you shouldn’t remove the whole infusion set, as the epinephrine that was in the tubing would go to waste.
Step 2: So after the tubing is removed from the cannula, a new infusion set should be opened. The needle cover should be removed, and the cannula sticker should be removed. The infusion set tubing should also be onwinded and the infusion set should be popped back to be ready for placement.
Step 3: When you have cleaned and secured your new site, push the button on the capsule, which will attach your new infusion set to your body.
Step 4: If you just changed your cartridge, to help conserve epinephrine, remove the new tubing that came with the new infusion set and attach your old tubing filled with epinephrine to the new cannula. If you're just changing your cartridge or changing it in the next twelve hours, remove your old tubing from the pump and attach the new tubing from the infusion set that's on your body directly to the pump.
Source: Reynolds, Roni. “How to Change Tandem Insulin Pump Cartridge and Infusion Set.” YouTube, 28 April 2021, https://www.youtube.com/watch?v=ZcQB2Ql90Ik. Accessed 11 March 2024.
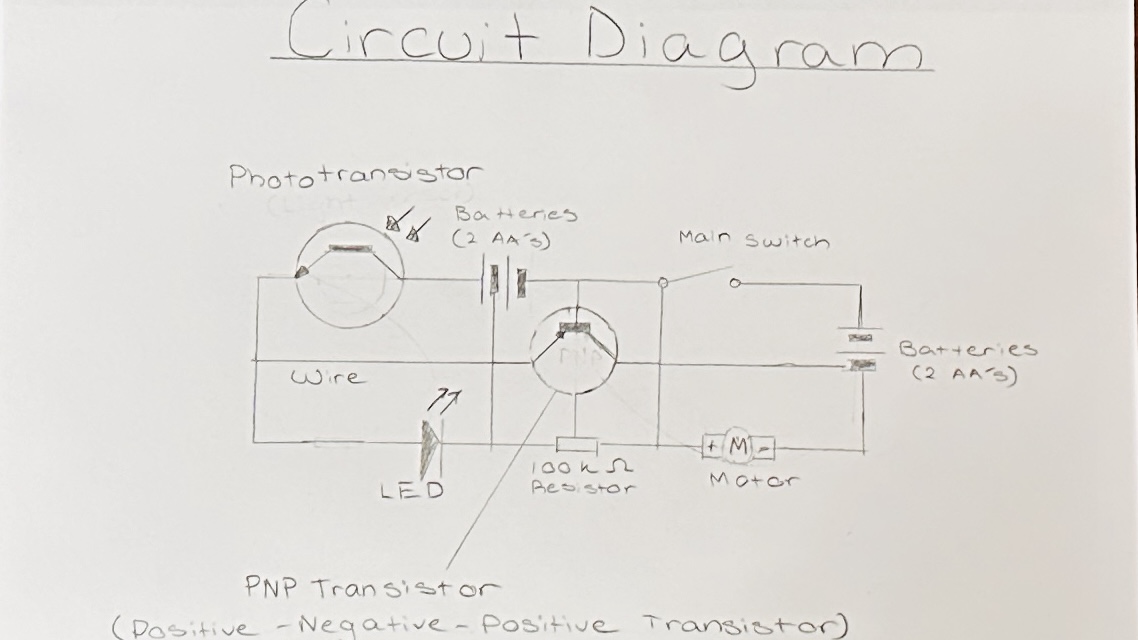
How the circuit works
The intuitive circuit was made to roughly represent the EpiPump functions through the use of a phototransistor, LED, and motor. The phototransistor represented the photodiodes in the Apple Watch sensor, and it functioned through sensing light or darkness. This phototransistor functioned when light was not sensed, meaning that it was darkness-activated. This darkness-activated sensor was used to represent the passing of the histamines in the artery. As the sensor detected darkness, the circuit was closed and the LED lit up. The LED in the circuit represented the functioning of the PCB in the EpiPump, beginning to activate the motor above it. The motor represented the motor in the EpiPump turning to release the epinephrine into the cannula and the patient's body.
https://drive.google.com/file/d/1QIxiedXYeTeiiltx0K7LvS9t_NWwZ54e/view?usp=sharing
Analysis
Our project's purpose is to design a machine that helps treat symptoms that may lead to anaphylaxis. Though there is already an Epipen to do this, we intend to help create a more reliable solution to treating anaphylaxis through the creation of the design of the EpiPump.
Our design is based on a tubed insulin pump and will have all the same internal and external components excluding 2 differences. Our design would pump a dose of epinephrine rather than a set rate of insulin. The sensors in the monitor will also be different as they would consist of fluorescent, chemical, and optical heart sensors, as they would be meant to detect symptoms of anaphylaxis.
Although the design idea is quite feasible, some potential shortcomings stand in the way of us fully creating it.
Successes:
- Based on our research, a responsive EpiPump can be built with a low cost by adopting the technology and materialsused in other similar systems like the insulin pump. The materials will most specifically be based off the "Ultra Low Cost Insulin Pump" by NIH. gov
- With sensor based EpiPumps that can trigger and pump epinephrine based on signs of anaphylaxis, hospitalization of patients and deaths can be greatly averted there by reducing expensive medical treatments for patients and freeing up medical resources for others.
These are:
- Our design. Our first design idea was based on a tubeless insulin pump, but soon after further research was done, we realized this was not the best decision because the tubeless insulin pump did not seem very buildable with the materials and resources we could acquire. The second problem was that the knowledge needed was way above our level of understanding, making us unable to cope with some of the instructions and code needed. The third problem was this design was made with all the parts very condensed together, making it harder to build a model that could function. To resolve these problems, we changed our design to a normal insulin pump that has a tube. This design seemed much more level to our understanding and seemed more buildable as the internal parts were more laid out, giving us an easier idea to build our design.
- The usage of code. We have not yet created a code for the EpiPump to function, which may be the biggest obstacle to producing it. However, the code that is used by insulin pumps has an extreme number of similarities to the potential code required to make the EpiPump function. Currently, the existing code that could be used for the EpiPump could be based on the code in the link at the bottom of the page, but with a few changes to accommodate the sensor functions and the contact of 911 during usage.
-
The type of technology we require to detect histamines. Fluorescent, Chemical, and Optical Heart sensors are all difficult to find in the market, so this is another shortcoming in the design of this device. Since we also have close to no experience dealing with these kinds of technology, our knowledge also limits us. To help resolve this, we decided to use a light-sensing diode to help represent the signal when our EpiPump monitor detects symptoms of anaphylaxis.
- The sensor's potential malfunction. Since our knowledge on the matter of the sensors is limited to only knowing how they work, we do know that they could potentially malfunction and make false readings, or not get readings at all. Currently, the best way to avert this type of situation is to take care of the sensors properly not damage them, and place them near the major arteries for optimal histamine detection. The worst-case scenario could involve using a spare EpiPen if it does not work.
- Any form of mechanical malfunction. To prevent parts of the EpiPump from malfunctioning, an internal look at the mechanisms annually or sooner can be done to make sure that all is still running well. As the mechanical parts in our design are very similar to insulin pump parts, our design can be reparable by contacting or asking someone who has a background in insulin pump technology to repair it.
- Batteries. The EpiPump design included 2 main AA batteries, but if the efficiency of the batteries and their lifetime reduces and causes less than optimal function, the battery source can be changed to a rechargeable lithium-ion battery. Using this will also make the design similar to other commercial insulin pumps and all iPhones today, and could potentially increase the lifespan of the insulin pump. A similar battery could be used for the sensor as well, to ensure optimal function and no shutdown during histamine detection. For more convenience, a part of the software could be dedicated to alerting the user of the EpiPump when the EpiPump and the sensor are low on battery. When this happens, the user will be encouraged to recharge the EpiPump before it runs completely out of charge.
- Epinephrine expiry and needle change for cannula. A solution for this could be logging the time the user inserts the new epinephrine into the EpiPump and the next time the user uses a needle. The pump can tell the user when it is time to get new epinephrine, and when to change the needle, usually in 2-3 weeks. But, the needle patch can potentially stay for 3 weeks longer than that.
Link to code from open source ultra-low cost insulin pump:https://data.mendeley.com/datasets/xb4tykn5gd/1
With a few altercations, this code can be used for the EpiPump as well, due to its uncanny similarities in function to insulin pumps.
Source: “Design of an open source ultra-low-cost insulin pump.” NCBI, 15 November 2022, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9679028/. Accessed 25 February 2024.
Matthew Payne, BA, University of Canterbury, provided this code from the above source as an alternative low-cost insulin pump that can be made in a normal household with inexpensive materials. It can be reproduced and test results from usage have been comparable to the accuracy of a commercial insulin pump, so this code could be used for best results.
Conclusion
We see the dangers of anaphylactic shock and without urgent treatment how it can be catastrophic. Our project aims to address problems that can occur when using an EpiPen incorrectly and thereby demonstrate the possibility of an alternative to the EpiPen. This proposed solution avoids dependency on the person going through anaphylaxis shock to administer an EpiPen themselves. It also avoids dependency on others to know how to administer an EpiPen.
Our proposed alternative of an Auto-deploying EpiPen drastically reduces the risk of death due to incorrect or untimely usage or dosage of Epinephrine during an anaphylactic shock.
Although it may come with some shortcomings, the feasibility and the possible accuracy of dosage has a high potential for creation, and assurance that there is little to no errors when dosed with epinephrine.
Citations
Wikipedia, https://www.google.com/url?sa=i&url=https%3A%2F%2Ftopas.com%2Fcompany%2Fnews%2Ftandems-wearable-insulin-pumps-utilize-topas-coc%2F&psig=AOvVaw3HokxJGNjei4aaKGhmHSE7&ust=1705977883480000&source=images&cd=vfe&opi=89978449&ved=0CBQQ3YkBahcKEwjYs-2Q_e-DAxUAAAA. Accessed 25 February 2024.
Aleppo, Grazia. “Insulin Pump: What to Know Before You Disconnect.” HealthCentral, https://www.healthcentral.com/condition/diabetes/how-disconnect-pump-plus-tips-traveling-pump-using-pump-school. Accessed 25 February 2024.
Allen, Jenn. “Type 1 diabetics say something is missing from Manitoba's new program to cover insulin pumps for young adults.” CBC, 5 August 2022, https://www.cbc.ca/news/canada/manitoba/manitoba-diabetic-insulin-pump-1.6541879. Accessed 25 February 2024.
“Anaphylaxis: Causes, Symptoms, Diagnosis & Treatment.” Cleveland Clinic, 17 October 2023, https://my.clevelandclinic.org/health/diseases/8619-anaphylaxis. Accessed 25 February 2024.
“Continuous Glucose Monitoring - NIDDK.” National Institute of Diabetes and Digestive and Kidney Diseases, https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes/continuous-glucose-monitoring. Accessed 25 February 2024.
“Design of an open source ultra low cost insulin pump.” NCBI, 15 November 2022, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9679028/. Accessed 25 February 2024.
“5 emergency steps - for treating anaphylaxis.” Food Allergy Canada, https://foodallergycanada.ca/wp-content/uploads/5-emergency-steps-for-treating-anaphylaxis.pdf. Accessed 25 February 2024.
“Histology, Mast Cells - StatPearls.” NCBI, https://www.ncbi.nlm.nih.gov/books/NBK499904/. Accessed 25 February 2024.
“How EpiPen® works.” Epipen.ca, https://www.epipen.ca/how-epipen-works. Accessed 25 February 2024.
Karra, Laila, and Francesca Levi. “Mast Cell Biology: Introduction and Overview - PMC.” NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3398748/. Accessed 25 February 2024.
“Main parts of an insulin pump. | Download Scientific Diagram.” ResearchGate, https://www.researchgate.net/figure/Main-parts-of-an-insulin-pump_fig3_44853030. Accessed 25 February 2024.
“Mast Cells – Cells and Smears.” Cells and Smears, 22 March 2018, https://vetclinpathimages.com/2018/03/22/mast-cells/. Accessed 25 February 2024.
“Monitor your heart rate with Apple Watch.” Apple Support, 21 September 2023, https://support.apple.com/en-ca/HT204666. Accessed 25 February 2024.
Smolinska, Sylwia. “Metabolites | Free Full-Text | Histamine: A Mediator of Intestinal Disorders—A Review.” MDPI, 10 December 1989, https://www.mdpi.com/2218-1989/12/10/895. Accessed 25 February 2024.
Surtini, Rusty. “,.” , - YouTube, 6 May 2021, https://pubs.acs.org/doi/10.1021/cr400546e. Accessed 25 February 2024.
“Tandem t: lock Cartridge.” Diabetes Express, https://diabetesexpress.ca/products/tandem-t-lock-cartridge. Accessed 25 February 2024.
“Food allergies.” WikiLectures, 1 November 2023, https://www.wikilectures.eu/w/Food_allergies. Accessed 2 March 2024.
“Anaphylaxis: Causes, Symptoms, Diagnosis & Treatment.” Cleveland Clinic, 17 October 2023, https://my.clevelandclinic.org/health/diseases/8619-anaphylaxis. Accessed 2 March 2024.
“File:Medtronic Paradigm 754.front.ajb.jpg.” Wikipedia, 2012, https://en.m.wikipedia.org/wiki/File:Medtronic_Paradigm_754.front.ajb.jpg. Accessed 3 March 2024.
Bartuzi, Zbigniew. “Figure 3. Percentage of the anaphylactic shock with and without a loss...” ResearchGate, https://www.researchgate.net/figure/Percentage-of-the-anaphylactic-shock-with-and-without-a-loss-of-consciousness-in-the_fig3_276423025. Accessed 14 March 2024.
Acknowledgement
We are exponentially grateful for the support of our parents and teachers in helping our project succeed, by providing both materials and valuable information for the science fair. We also thank Jake Halle for helping us develop our project idea.